The Patient Safety Digest

Prescribing Patterns Indicate Risk of Medication Error
Are you crazy?!? This IV Calcium order is totally wrong! Are you trying to kill the patient?!? The nurse was right, of course… The medical order I entered into the EMR was totally wrong and could have caused significant harm to the patient. Luckily for the patient (and for me), the nurse caught the error right away, but it was a close call. This was the first time I ordered a concentrated high-dose calcium infusion, and even though I read the instructions before writing the order, I still got it wrong…
Was it because it was the first time I wrote such an order? Was it related to the fact that it was 2am in the morning or that the ER was packed with screaming patients? Maybe, but it was me who almost harmed the patient and everything else is just excuses.
Studies show medication safety issues result in more than 1.5 million patients harmed and hundreds of thousands of deaths annually. In order to improve medication safety, it is important to first understand the root causes of the problem.
My colleagues and I recently participated in a study published by the Journal of American Medical Informatics Association (JAMIA) focused on the many causes of prescription errors. While there are a number of technical factors that can lead to prescription errors, the research identified one of the leading physician-related causes of prescription errors was experience prescribing the specific medication.
Practice and Medication Inexperience Causes Prescription Errors
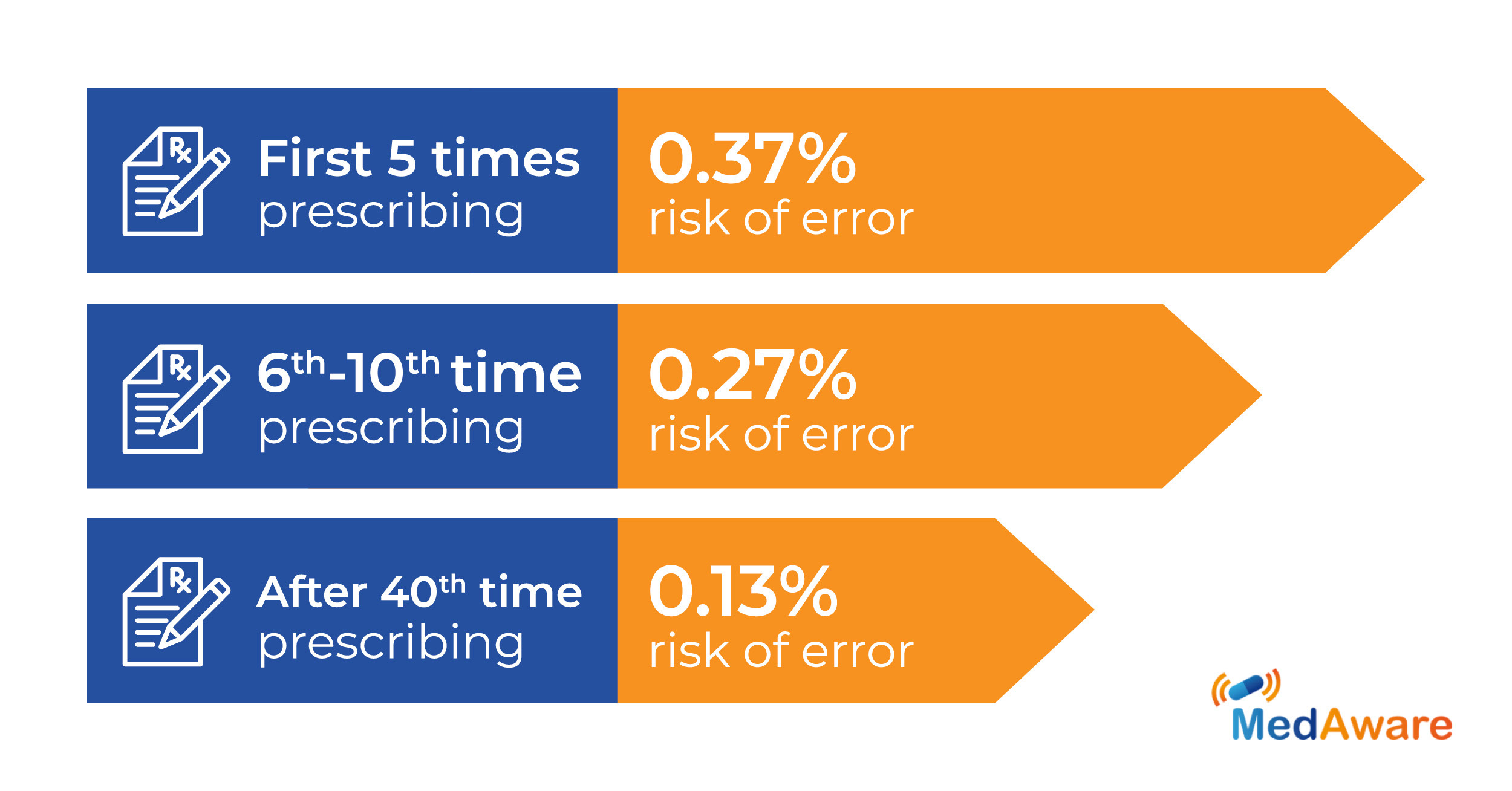
It seems rational to imagine that physicians who are more experienced with a specific medication make less prescribing errors. When a less experienced physician prescribes a medication they are unfamiliar with or “naive” to, they are three times as likely to err compared to prescribers with more experience with the medication. Nearly half—46 percent— of the medication-related errors found in the JAMIA study were caused by “naive” physicians who had prescribed the drug less than five times.
As expected, when a physician becomes more familiar with the medication, their risk of error decreases. For a physician who has prescribed a medication over 40 times, the risk of error is only 0.13 percent. Yet for a physician writing a prescription for the first 6-10 scripts, the JAMIA study found errors occurred 0.27 percent of the time.
Unfortunately, this inexperience has only risen since the study concluded. Due to the increased demand during the pandemic, many residents and physicians in other disciplines have been redeployed to the ICU ill-equipped and with very little ICU experience. Due to the rapid increase in hospital cases, these changes occurred with little warning—making it difficult for hospitals to appropriately train healthcare workers on their new responsibilities.
Interestingly, overall medical inexperience didn’t have a significant correlation with an increased rate of prescription errors. The risk to err was 0.16 percent in the first six months of employment and decreased to 0.10 percent after two years.
Creating Provider-Specific Medication Safety Nets
Moving forward to prevention, ongoing monitoring of prescribing behavior can identify opportunities for increased training to help improve a provider’s experience level with those medications and ultimately diminish the risk of future error. As new clinical tools move towards a more personalized approach, the focus needs to be on both patient history AND provider history and experience.
Unfortunately, existing clinical decision support (CDS) does not factor in physician experience when generating medication safety warnings. Rules-based drug interaction databases generate alerts based mainly on dosage outliers and drug-drug interactions without factoring in the experience of the physician working with a specific drug. Generating the same amount and degree of alerts for physicians prescribing a medication for the first time and for the hundredth time results in alert fatigue that renders these alerts ineffective.
Instead, a clinician-enabled medication safety solution could know how many times a prescriber has ordered a specific medication. If the prescriber has never ordered or prescribed that medication before, the tool searches for more specific errors and presents personalized, relevant alerts. This approach can also better identify when a physician prescribes the wrong medication by mistake.
Not only will the CDS monitor a physician’s naivety of a new drug prescription, but the pharmacist will serve as an extra layer of protection within the matrix of the patient’s medication safety net. Smart CDS can focus the attention of the pharmacist to evaluate and prioritize risk based on the doctor’s experience with the drug in question, combined with the longitudinal patient profile, and identify mistakes before they cause harm.
This technology can monitor outliers in physician behavior, as well as patient behavior patterns in order to reduce prescription errors to a minimum. Understanding prescriber patterns to see if additional support is needed when prescribing a medication the physician doesn’t normally work with helps improve outlier detection and increases the value of CDS.
For more information on the relationship between physician experience and medication errors, download our eBook. See even further insights and interpretations of prescription error data and learn how personalized, clinician-driven AI (artificial intelligence) can help.
Related Articles
Look-Alike, Sound-Alike Medications Get an AI-Assist to Improve Patient Safety
According to a 2019 report from the Institute for Safe Medication Practices (ISMP), there are...How MedAware Supports ISMP’s Newest Medication Best Practices
Recently, the Institute for Safe Medication Practices issued three new best practices for targeted...US Toll Free:+1-800-280-3040
ISRAEL:+972-9-740-4939

